I am a researcher in the Department of Human Oncology. My primary focus is on brachytherapy—the treatment of disease using radiation over short distances, primarily using radioactive materials. I am responsible for the treatment planning, safety and administration of brachytherapy procedures at the University of Wisconsin Hospital. My previous role in the department was oversight of the TomoTherapy program from 2008 to 2010. Since joining the department in 2007, I have been responsible for the education of radiation physics residents and radiation therapy interns with regard to brachytherapy. My research focus includes improvement in MR/CT imaging for brachytherapy and improved administration and treatment planning methods for brachytherapy. I currently serve on the Human Radiation Use Committee (HRUC).
Education
MS, University of Wisconsin–Madison, Medical Physics (2007)
BS, Michigan State University, Physics (2005)
Academic Appointments
Researcher, Human Oncology (2017)
Associate Researcher, Human Oncology (2013)
Assistant Researcher, Human Oncology (2007)
Boards, Advisory Committees and Professional Organizations
American Association of Physicists in Medicine, Member (2005–pres.)
Diplomate of The American Board of Radiology (DABR), Therapeutic Medical Physics (2011)
Charles Wallace is responsible for the treatment planning, safety and administration of brachytherapy procedures at the University of Wisconsin Hospital. His research focuses on improving MR/CT imaging and administration and treatment planning methods for brachytherapy. He currently serves on the Human Radiation Use Committee.
Improving accuracy of brachytherapy treatment delivery
Brachytherapy treatment is only accurate if the imaging performed of the applicator with respect to the patient closely approximates the geometry of the actual treatment. This can be realized with improved imaging techniques, management of patient motion, better workflow to reduce total procedure time and robust treatment planning techniques.
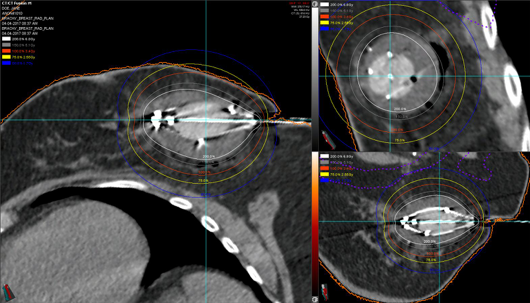
For nearly two decades, balloon-based high dose-rate applicators for irradiation of breast lumpectomy cavities has been an effective treatment for women with early-stage breast cancer. Recently, our institution developed a novel double-balloon applicator that allows for a customizable distance of the radiation source from the breast tissue. However, this customizability may potentially result in dose distributions that could under-cover the target or cause unnecessarily high dose to normal tissue if the applicator is rotated from its intended position. The focus of this research is to assess the potential impact of rotation of the balloon during treatment and develop treatment planning methods that will minimize this discrepancy in the case of rotation without compromising target coverage.
-
Dosimetric evaluation of adaptive planning for five-fraction gynecologic template-based interstitial brachytherapy Brachytherapy
Blum S, Miller JR, Bradley KA, Anderson B, Menon H, Eckelmann B, Wallace C, Besemer A, Lawless M, Slagowski JM
2024 Nov-Dec;23(6):668-675. doi: 10.1016/j.brachy.2024.07.007. Epub 2024 Aug 31.
-
More
PURPOSE: The purpose of this work was to evaluate whether inter-fraction imaging and replanning enhance treatment delivery adherence to clinical planning objectives in the context of a 5-fraction template-based interstitial brachytherapy (TISB) approach for gynecologic cancer treatment.
METHODS AND MATERIALS: This retrospective study analyzed nineteen patients who underwent 5 fractions of interstitial brachytherapy over 3 days using the Syed-Neblett template. A verification CT scan was acquired for applicator assessment and reviewed by a radiation oncologist and medical physicist before each fraction. Eleven patients required replanning at least once during the treatment course. Replanning on the verification CT scan consisted of generating new target and organ-at-risk contours, digitizing catheter positions, and optimizing source dwell times to meet planning objectives. Dwell times and positions from the initial treatment plan were evaluated on the new contours to assess the dose that would have been delivered without replanning (nonadapted). Significance of nonadapted versus adapted dose differences were evaluated using a 2-sided Wilcoxon sum rank test.
RESULTS: The average (min, max) change in dose (Gy) between the clinically delivered plans and the nonadapted plans were HR-CTV D90%: -6.5 (-0.6, -15.1), HR-CTV D98%: -6.5 (-0.4, -12.6), Bladder D2cc: -0.5 (0.0, -2.8), Bowel D2cc: -0.8 (0.0, -3.2), Rectum D2cc: -1.1 (0.0, -11.5), Sigmoid D2cc: -1.4 (-0.1, -5.4). Dosimetric changes in HR-CTV coverage were significantly improved with replanning while organ-at-risk differences were nonsignificant (p > 0.05). Fraction 3 was the most common fraction indicated for replanning.
CONCLUSIONS: Replanning template-based interstitial brachytherapy can improve target coverage and adherence to planning goals.
PMID:39217003 | DOI:10.1016/j.brachy.2024.07.007
View details for PubMedID 39217003
-
More
-
Interstitial Brachytherapy for Lip Cancer: Technical Aspects to Individualize Treatment Approach and Optimize Outcomes Practical radiation oncology
Merfeld EC, Witek ME, Francis DM, Burr AR, Wallace CR, Kuczmarska-Haas A, Lamichhane N, Kimple RJ, Glazer TA, Wieland AM, McCulloch TM, Hartig GK, Harari PM
2023 Jul-Aug;13(4):340-345. doi: 10.1016/j.prro.2023.01.004. Epub 2023 Jan 25.
-
More
Primary radiation therapy using interstitial brachytherapy (IBT) provides excellent local tumor control for early-stage squamous cell carcinoma of the lip. Technical aspects of treatment are important to optimize outcomes. In this report, we discuss patient selection criteria, procedural details, and dosimetric considerations for performing IBT for cancers of the lip. Catheters are inserted across the length of tumor entering and exiting approximately 5 mm beyond the palpable tumor extent. A custom mouthpiece is fabricated to facilitate normal tissue sparing. Patients undergo computed tomography imaging, the gross tumor volume is contoured based on physical examination and computed tomography findings, and an individualized brachytherapy plan is generated with the goals of achieving gross tumor volume D90% ≥ 90% and minimizing V150%. Ten patients with primary (n = 8) or recurrent (n = 2) cancers of the lip who received high-dose-rate lip IBT using 2.0- to 2.5-week treatment regimens are described (median prescription: 47.6 Gy in 14 fractions of 3.4 Gy). Local tumor control was 100%. There were no cases of acute grade ≥4 or late grade ≥2 toxicity, and cosmesis scores were graded as good to excellent in all patients. IBT represents an excellent treatment option for patients with lip squamous cell carcinoma. With careful attention to technical considerations furthered described in the present report, high rates of tumor control, low rates of toxicity, and favorable esthetic and functional outcomes can be achieved with IBT for lip cancer.
PMID:36709044 | PMC:PMC10330101 | DOI:10.1016/j.prro.2023.01.004
View details for PubMedID 36709044
-
More
-
Targeting the GTV in medically inoperable endometrial cancer using brachytherapy Brachytherapy
Merfeld EC, Kuczmarska-Haas A, Burr AR, Witt JS, Francis DM, Ntambi J, Desai VK, Huang JY, Miller JR, Lawless MJ, Wallace CR, Anderson BM, Bradley KA
2022 Nov-Dec;21(6):792-798. doi: 10.1016/j.brachy.2022.07.006. Epub 2022 Aug 24.
-
More
PURPOSE: We aimed to determine the relationship between gross tumor volume (GTV) dose and tumor control in women with medically inoperable endometrial cancer, and to demonstrate the feasibility of targeting a GTV-focused volume using imaged-guided brachytherapy.
METHODS AND MATERIALS: An endometrial cancer database was used to identify patients. Treatment plans were reviewed to determine doses to GTV, clinical target volume (CTV), and OARs. Uterine recurrence-free survival was evaluated as a function of CTV and GTV doses. Brachytherapy was replanned with a goal of GTV D98 EQD2 ≥ 80 Gy, without regard for coverage of the uninvolved uterus and while respecting OAR dose constraints.
RESULTS: Fifty-four patients were identified. In the delivered plans, GTV D90 EQD2 ≥ 80 Gy was achieved in 36 (81.8%) patients. Uterine recurrence-free survival was 100% in patients with GTV D90 EQD2 ≥ 80 Gy and 66.7% in patients with EQD2 < 80 Gy (p = 0.001). On GTV-only replans, GTV D98 EQD2 ≥ 80 Gy was achieved in 39 (88.6%) patients. Mean D2cc was lower for bladder (47.1 Gy vs. 73.0 Gy, p < 0.001), and sigmoid (47.0 Gy vs. 58.0 Gy, p = 0.007) on GTV-only replans compared to delivered plans. Bladder D2cc was ≥ 80 Gy in 11 (25.0%) delivered plans and four (9.1%) GTV-only replans (p = 0.043). Sigmoid D2cc was ≥ 65 Gy in 20 (45.4%) delivered plans and 10 (22.7%) GTV-only replans (p = 0.021).
CONCLUSIONS: OAR dose constraints should be prioritized over CTV coverage if GTV coverage is sufficient. Prospective evaluation of image-guided brachytherapy to a reduced, GTV-focused volume is warranted.
PMID:36030167 | DOI:10.1016/j.brachy.2022.07.006
View details for PubMedID 36030167
-
More
-
Low cardiac and left anterior descending coronary artery dose achieved with left-sided multicatheter interstitial-accelerated partial breast irradiation Brachytherapy
Witt JS, Gao RW, Sudmeier LJ, Rosenberg SA, Francis DM, Wallace CR, Das RK, Anderson BM
2019 Jan-Feb;18(1):50-56. doi: 10.1016/j.brachy.2018.08.014. Epub 2018 Sep 24.
-
More
PURPOSE: Studies have shown that an additional mean dose of 1 Gy to the heart can increase the relative risk of cardiac events. The purpose of this study was to quantify the dose delivered to the heart and left anterior descending artery (LAD) in a series of patients with left-sided breast cancer (BC) or ductal carcinoma in situ treated with multicatheter-accelerated partial breast irradiation (MC-APBI) at a single institution.
METHODS AND MATERIALS: Patients with left-sided BC or ductal carcinoma in situ treated consecutively from 2005 to 2011 with MC-APBI were retrospectively identified. Cardiac and LAD contours were generated for each patient. Cardiac dosimetry and distance to the planning target volume were recorded. Patient health records were reviewed and cardiac events were recorded based on Common Terminology Criteria for Adverse Events version 4.0.
RESULTS: Twenty consecutive patients with left-sided BC treated with MC-APBI were retrospectively identified. Median followup was 41.4 months. Mean equivalent dose in 2 Gy fractions delivered to the heart and LAD were 1.3 (standard deviation: 0.7, range: 0.2-2.9) and 3.8 (standard deviation: 3.0, range: 0.4-11.3) Gy, respectively. There was an inverse linear relationship (R2 = 0.52) between heart-to-lumpectomy cavity distance and mean heart equivalent dose in 2 Gy fractions. One patient (5%) experienced symptomatic cardiac toxicity.
CONCLUSIONS: MC-APBI consistently delivers average doses to the heart and LAD that are similar to those achieved in most series with deep inspiration breath-hold and lower than free-breathing radiotherapy techniques. Distance from the heart to the lumpectomy cavity and the availability of other heart-sparing technologies should be considered to minimize the risk of cardiac toxicity.
PMID:30262411 | PMC:PMC6338487 | DOI:10.1016/j.brachy.2018.08.014
View details for PubMedID 30262411
-
More
-
Novel use of ViewRay MRI guidance for high-dose-rate brachytherapy in the treatment of cervical cancer Brachytherapy
Ko HC, Huang JY, Miller JR, Das RK, Wallace CR, Costa AD, Francis DM, Straub MR, Anderson BM, Bradley KA
2018 Jul-Aug;17(4):680-688. doi: 10.1016/j.brachy.2018.04.005. Epub 2018 Jun 7.
-
More
PURPOSE: To characterize image quality and feasibility of using ViewRay MRI (VR)-guided brachytherapy planning for cervical cancer.
METHODS AND MATERIALS: Cervical cancer patients receiving intracavitary brachytherapy with tandem and ovoids, planned using 0.35T VR MRI at our institution, were included in this series. The high-risk clinical target volume (HR-CTV), visible gross tumor volume, bladder, sigmoid, bowel, and rectum contours for each fraction of brachytherapy were evaluated for dosimetric parameters. Typically, five brachytherapy treatments were planned using the T2 sequence on diagnostic MRI for the first and third fractions, and a noncontrast true fast imaging with steady-state precession sequence on VR or CT scan for the remaining fractions. Most patients received 5.5 Gy × 5 fractions using high-dose-rate Ir-192 following 45 Gy of whole-pelvis radiotherapy. The plan was initiated at 5.5 Gy to point A and subsequently optimized and prescribed to the HR-CTV. The goal equivalent dose in 2 Gy fractions for the combined external beam and brachytherapy dose was 85 Gy. Soft-tissue visualization using contrast-to-noise ratios to distinguish normal tissues from tumor at their interface was compared between diagnostic MRI, CT, and VR.
RESULTS: One hundred and forty-two fractions of intracavitary brachytherapy were performed from April 2015 to January 2017 on 29 cervical cancer patients, ranging from stages IB1 to IVA. The median HR-CTV was 27.78 cc, with median D90 HR-CTV of 6.1 Gy. The median time from instrument placement to start of treatment using VR was 65 min (scan time 2 min), compared to 105 min using diagnostic MRI (scan time 11 min) (t-test, p < 0.01). The contrast-to-noise ratio of tumor to cervix in both diagnostic MRI and VR had significantly higher values compared to CT (ANOVA and t-tests, p < 0.01).
CONCLUSIONS: We report the first clinical use of VR-guided brachytherapy. Time to treatment using this approach was shorter compared to diagnostic MRI. VR also provided significant advantage in visualizing the tumor and cervix compared to CT. This presents a feasible and reliable manner to image and plan gynecologic brachytherapy.
PMID:29773331 | DOI:10.1016/j.brachy.2018.04.005
View details for PubMedID 29773331
-
More
-
Clinical implementation of a novel Double-Balloon single-entry breast brachytherapy applicator Brachytherapy
Anderson BM, Wallace CR, Costa AD, Das RK
2017 Nov-Dec;16(6):1239-1245. doi: 10.1016/j.brachy.2017.07.015. Epub 2017 Aug 24.
-
More
PURPOSE: The purpose of the study was to describe the clinical utilization of a novel Double-Balloon applicator for accelerated partial breast irradiation (APBI).
METHODS AND MATERIALS: The Double-Balloon single-entry breast applicator contains a single central treatment catheter, as well as four peripheral catheters that can be differentially loaded to customize radiation dose coverage. An inner balloon is filled with up to 7-30 cm3 of saline to increase separation between the peripheral catheters, and an outer balloon is filled with up to 37-115 cm3 of saline to displace breast tissue from the peripheral catheters. Treatment planning objectives include coverage of the breast planning target volume to a minimum of V90 > 90%, limiting dose heterogeneity such that V200 < 10 cm3 and V150 < 50 cm3, and limiting maximum dose to skin (<100% of prescription dose) and ribs (<145% of prescription dose).
RESULTS: High-dose-rate APBI was delivered to 11 women using this device (34 Gy in 10 twice daily fractions). The mean V90 was 98.2% (range 94.2-99.4%). The mean skin Dmax with the Double-Balloon applicator was 83.3% (range 75.6-99.5%). The mean breast V200 was 5.8 cm3 (range 2.3-10.2 cm3), and the mean breast V150 was 32.9 cm3 (range 25.0-41.7 cm3). Pretreatment quality assurance was performed using CT prior to each morning fraction and ultrasound prior to each afternoon fraction.
CONCLUSIONS: The Double-Balloon applicator can be easily introduced into a previously existing brachytherapy program. APBI plans created with this applicator achieve excellent planning target volume coverage, while limiting skin dose and maintaining breast V200 < 10 cm3.
PMID:28844820 | DOI:10.1016/j.brachy.2017.07.015
View details for PubMedID 28844820
-
More
-
Technical Note: Confirming the prescribed angle of CT localizer radiographs and c-arm projection acquisitions Medical physics
Szczykutowicz TP, Labby ZE, Rubert N, Wallace C
2016 Feb;43(2):865-9. doi: 10.1118/1.4940124.
-
More
PURPOSE: Accurate CT radiograph angle is not usually important in diagnostic CT. However, there are applications in radiation oncology and interventional radiology in which the orientation of the x-ray source and detector with respect to the patient is clinically important. The authors present a method for measuring the accuracy of the tube/detector assembly with respect to the prescribed tube/detector position for CT localizer, fluoroscopic, and general radiograph imaging using diagnostic, mobile, and c-arm based CT systems.
METHODS: A mathematical expression relating the x-ray projection of two metal BBs is related to gantry angle. Measurement of the BBs at a prescribed gantry (i.e., c-arm) angle can be obtained and using this relation the prescribed versus actual gantry angle compared. No special service mode or proprietary information is required, only access to projection images is required. Projection images are available in CT via CT localizer radiographs and in the interventional setting via fluorography.
RESULTS: The technique was demonstrated on two systems, a mobile CT scanner and a diagnostic CT scanner. The results confirmed a known issue with the mobile scanner and accurately described the CT localizer angle of the diagnostic system tested.
CONCLUSIONS: This method can be used to quantify gantry angle, which is important when projection images are used for procedure guidance, such as in brachytherapy and interventional radiology applications.
PMID:26843247 | DOI:10.1118/1.4940124
View details for PubMedID 26843247
-
More
Contact Information
Charles Wallace, MS
600 Highland Avenue Madison, Box 0600 Clinical Science Center,Madison, WI 53792