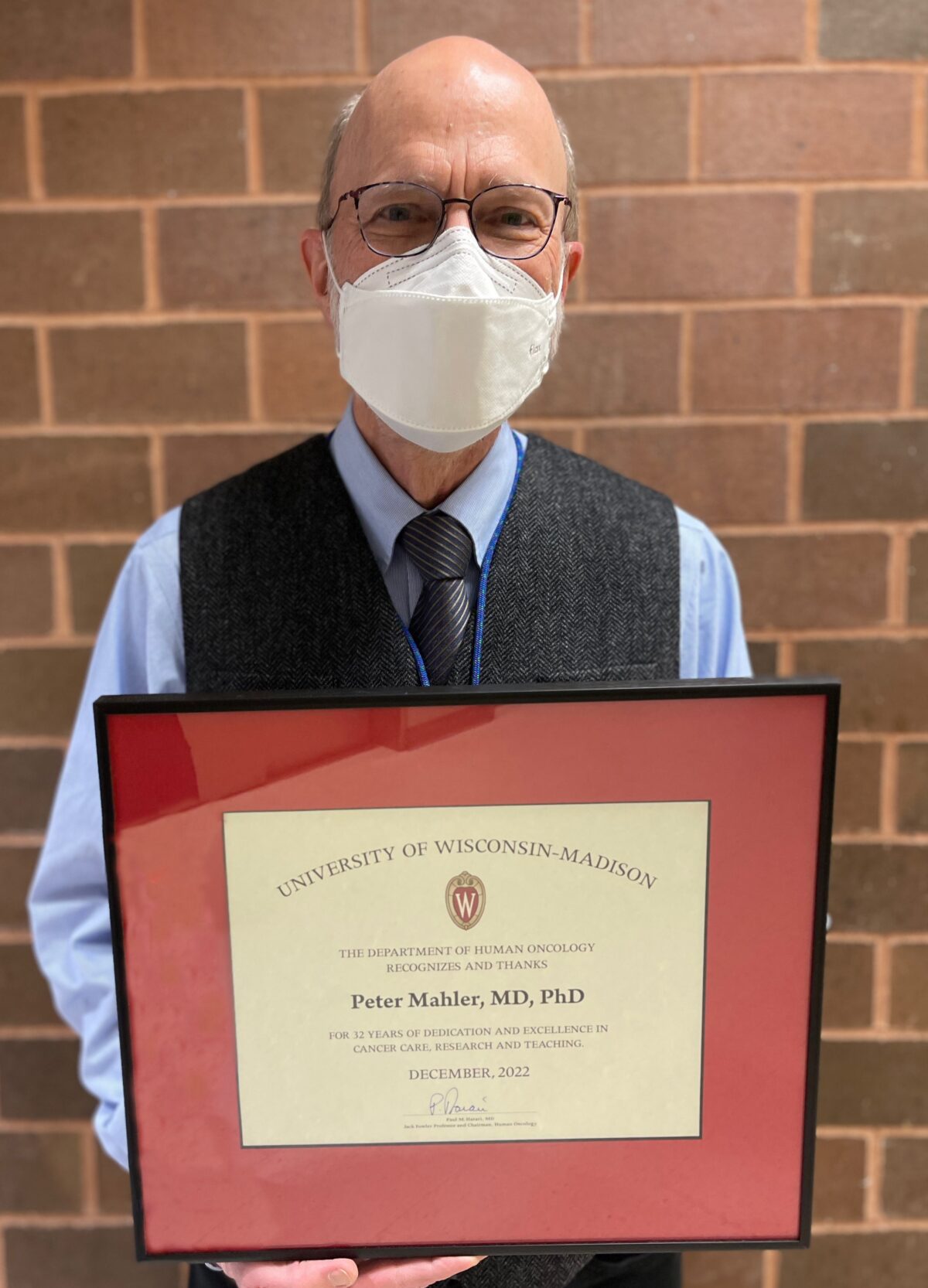
 Professor Peter Mahler, PhD, MD, Department of Human Oncology, retired on February 28, 2023 after a long association with the University of Wisconsin. His career has taken him from the Midwest to the Eastern Great Lakes to the West Coast and then back to Wisconsin.
Professor Peter Mahler, PhD, MD, Department of Human Oncology, retired on February 28, 2023 after a long association with the University of Wisconsin. His career has taken him from the Midwest to the Eastern Great Lakes to the West Coast and then back to Wisconsin.
He earned his PhD in Radiation Biology at the University of Rochester in NY, one of the original sites of the Manhattan Project during WWII. He then came to Madison in 1978 for a post-doctoral fellowship. In 1981 he went to the University of Washington in Seattle. While doing research in Seattle, he realized how much he enjoyed people and wanted to help them, so he went on to Medical School there. When he was finished, he returned to Madison completing his Internship and Residency in Radiation Oncology in 1991. After his residency, he stayed on at the UW Cancer Center. He told me that the Wisconsin Idea, the philosophy that activity at UW should help people’s lives beyond the boundaries of the university, played a part in his decision to stay here. With Professor Mahler‘s “people first” history, that is not surprising.
DHO: You received a bachelor’s degree in 1970 in Physics. How long have you been interested in using radiation therapeutically?
PM: Probably when I did my post-doc here.
 I earned a bachelor’s degree in physics and then did graduate work for a year at the University of Illinois. While at the U of I, I was introduced to the field of Radiation Biology, and after teaching physics for two years, I returned to graduate school, focusing on radiation biology, earning a PhD in 1978. At that point, my interest was how does radiation cause cancer. It was an area that needed to be better understood, and I decided on doing that. My rational was straight forward. People were worried about radiation from nuclear energy. Since wars are often fought over control of natural resources, I wondered, perhaps naively, if the likelihood of war could be reduced if we could create abundant energy from nuclear sources. To have that happen, we needed more information on the risks of radiation induced cancer. Therefore, my PhD research dealt with the effects of radiation and hormone stress on the creation of thyroid cancer.
I earned a bachelor’s degree in physics and then did graduate work for a year at the University of Illinois. While at the U of I, I was introduced to the field of Radiation Biology, and after teaching physics for two years, I returned to graduate school, focusing on radiation biology, earning a PhD in 1978. At that point, my interest was how does radiation cause cancer. It was an area that needed to be better understood, and I decided on doing that. My rational was straight forward. People were worried about radiation from nuclear energy. Since wars are often fought over control of natural resources, I wondered, perhaps naively, if the likelihood of war could be reduced if we could create abundant energy from nuclear sources. To have that happen, we needed more information on the risks of radiation induced cancer. Therefore, my PhD research dealt with the effects of radiation and hormone stress on the creation of thyroid cancer.
I came to the UW-Madison for a postdoc in 1978, to work with Dr. Kelly Clifton, who was a radiation biologist in the Department of Human Oncology (DHO). The department was fairly new having been created in response to the National Cancer Act (NCA) of 1971, which funded cancer centers around the country. (As an aside, a major shaker and mover in getting the NCA passed was Mary Lasker, a Watertown WI native.) A comprehensive cancer center was created at the UW, recruiting faculty from the McArdle Cancer Center, and other campus and Medical School departments.
Dr. Clifton was doing research investigating how radiation causes breast cancer. At that time in particular, he wanted to study the effects of neutron radiation. I was the person brought in to do that. Part of my duties were putting rats from the hospital vivarium into cages, putting the cages into my VW bug, driving them to Stoughton where medical physics had a neutron facility, irradiating the rats, bringing them back here, putting them back in the animal facility, and doing research, trying to figure out how dangerous neutrons were compared to X-rays.
Dr. Milt Yatvin, who was another radiation biologist in DHO, someone with too many ideas and not enough people to work for him, got me to work on a project with him looking at the effect of dietary protein on radiation damage on normal kidneys.
The normal tissue work was interesting. When I went to the University of Washington as a new research faculty member, I began looking at lung damage from radiation – lung cancer causing the most cancer related deaths, then and still now. In particular, I studied vascular permeability changes, thinking that this contributed to radiation induced inflammation and post radiation lung scarring. I thought that if we could figure out how to make the normal tissue more tolerant of radiation, we could give more radiation, and increase the probability of eradicating a lung cancer.
While I was doing this research using rats, I was also collaborating with several physicians. They were caring for patients and doing research. At that point I came to the realization that I really liked people more than rats. I applied to medical school and received my medical degree in three years at the U of Washington in 1987.
I elected to return to UW-Madison for Residency. My wife and I had positive memories of living here and knew it would be a great place to raise our two young children. Another attraction was that the DHO had recruited a new chairman from the National Cancer Institute, who was supposed to be a fast-ascending star. In addition, the UW, had just started the School of Veterinary Medicine. I thought trying to combine veterinarians with radiation research, animal research, would be worthwhile.
So, I did residency here, finishing in 1991. There weren’t clinical openings on the main campus for a radiation oncologist but we had just started an affiliation with Beloit Memorial Hospital. Initially I had three days a week on campus to focus on research, two days of clinical work in Beloit. On campus I collaborated with Lisa Forest DVM, and David Vail DVM, evaluating lung damage from radiation in dogs, using CT scans and bronchoscopy.
With time it became, “well we needed you in Beloit three days a week. And four days a week and five days a week.” And so, for the last 20 plus years that I was at Beloit I had a five day a week commute, lived in Madison, went to Beloit, and then came back home. When I retired from Beloit, the medical oncologist calculated that my commutes all totaled, amounted to more driving than going to the moon and back. I enjoyed the patient contact and all the staff I worked with – caring people.
A story I like is that when I came from my postdoc, the current hospital building was being built. The radiation biologists had their labs where the old hospital is on University Avenue. When we moved out to our current site, we arrived several months before patients were moved. The idea was similar to a shakedown cruise – find out what works with the building and what doesn’t and so forth. So, I’ll claim fame to being one of the longest duration occupants of the building – here before patients – although I did have a six-year hiatus while I was in Seattle.
DHO: Anyone who’s had a friend or loved one with late-stage cancer understands the importance of palliative care. What initially made you interested in that?
PM: That’s a little bit of a funny story. I had been in Beloit, probably five, six years, maybe a little longer.
One day two women came to the radiation oncology area and asked, “Would you be a hospice medical director?” I said, “I don’t know much about hospice, and I don’t know anything about hearts. I don’t think I would be a good match for you.” And they said, “Well, that’s okay. We have another physician who’s a family practice doctor and she says she’s fine with hearts, but doesn’t know anything about cancer.” The story was that the Beloit medical oncologist had been a medical director for the hospice for years, but decided he didn’t want to do that anymore, and now they were looking for a replacement.
I said, “Okay, we’ll try it for three months. And if you don’t like me or I don’t like it, then we’ll stop.” I continued for almost 20 years and really enjoyed it. Hospice (and Palliative Care) are truly areas of team medicine, where much of the work is done by the nurses and aides and social workers and chaplains.
About 10 years ago, hospice and palliative care was an expanding entity, and it was decided to make it a board-certified part of medicine. But because hospice physicians traditionally had come from all types of medical specialties, the specialty of Hospice and Palliative Care (HPC) physicians without experience would require a one-year fellowship, followed by a board exam. Individuals who had been HPC physicians for years would be allowed to be certified if the passed the board exam. I thought, well that’s interesting, I’d be glad to do that. Then the “powers that be” stated, well you can be a surgeon, you can be an internist, you can be a family practice doc, you can be an OB-GYN, you can be an Anesthesiologist…….but they didn’t list Radiology or Radiation Oncology.
As Radiation Oncologists we deal with patients, we deal with cancer patients, we deal with pain and other symptoms. So, at one of the ASTRO (American Society for Radiation Oncology) meetings about that time, I happened to see the President of ASTRO. I didn’t know him personally, but when I saw him in the halls, I mentioned this to him. His response was, “Oh, so they don’t think Radiation Oncologists are physicians, eh? Well, let me look at that.”
I believe he talked to somebody, somewhere, and radiation oncologists were permitted to sit for the exam. I took it and earned board certification.
When I stopped going to Beloit full time, I spoke with Dr. Toby Campbell, Chief of Palliative Care here at the hospital. I asked “Toby, do you need any extra help?” And at that time, one of their primary palliative care doctors was gone for a few months, and so Toby said, “Yeah, we could use someone.”
I then was part of the inpatient palliative care team for two years. It was very rewarding, working with another great group of caring individuals. I think that fits in with the reason I went into medicine, and that is, the opportunity to help people.
My last clinical Radiation Oncology duties were at East Clinic and the UW-Johnson Creek Cancer Center, as a “utility infielder”, filling in as needed. Again, two great groups of caring team members – great radiation therapists, medical physicists, nurses, and support staff – , and another chance to be part of the Wisconsin Idea.
DHO: Do you have any general advice for students, new residents, and new faculty?
PM: I’ve often had someone say, “Oh, cancer, it’s terrible. Patients die, how can you do this work?” And I say, “Well, if your goal is to cure every patient, you’re going to be disappointed and frustrated. If your goal is to cure as many as you can and help every patient, that is achievable and rewarding.”
It is important to listen, to find out about other people. Enjoy people. I think that’s something I fortunately got from my parents.
When I have a new consult, one of my first questions is, “Tell me about yourself.” The rationale for that is pretty solid in terms of, if you know that person somewhat, you can communicate more effectively with them. Is this a skilled craftsman I am dealing with? Or is it somebody with a different background – a preschool teacher, or farmer, or college science professor, or airline pilot? And that was something, to my embarrassment, I had learned after years in Beloit.
Of a new consult, I asked: “What did you do after you finished high school?”
He replied, “I didn’t finish high school.”
He probably was embarrassed. I definitely was embarrassed. From then on, I’d ask, “What did you do after you finished going to school?”
One is never too old to learn.