
The American Society for Radiation Oncology (ASTRO) has been working to reduce restrictive prior authorization practices through legislative efforts and by raising awareness of the issue with key decision makers on Capitol Hill.
In September 2019, Dr. Paul Harari, ASTRO Chairman of the Board, testified before Congress on how prior authorization increasingly restricts physicians from exercising their clinical judgment in determining what is in the best interest of cancer patients. The prior authorization process can create unnecessary delays in treatment that harm cancer patient outcomes.
You can view Dr. Harari’s Congressional testimony here.
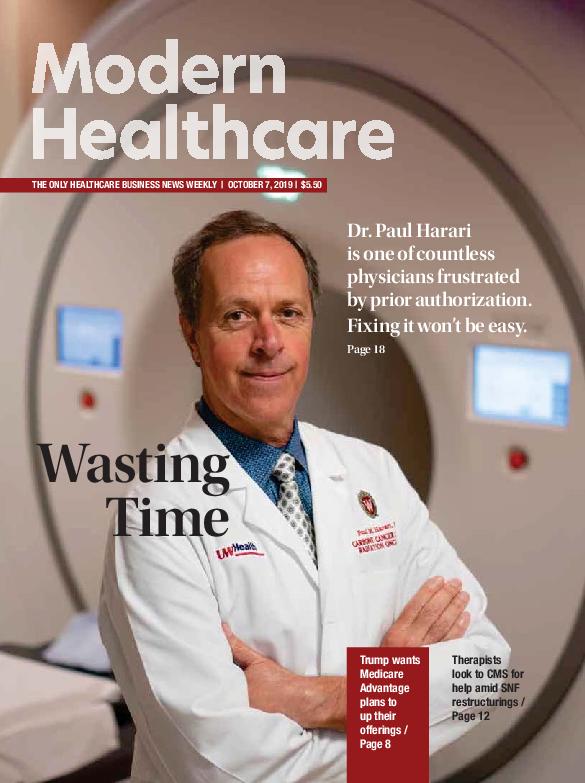
Following his testimony, Dr. Harari was featured on the cover of the Oct. 7 issue of Modern Healthcare.
The following is an excerpt from that article:
Momentum builds to fix prior authorization
Modern Healthcare – 10/5/19
Dr. Paul Harari, a radiation oncologist, likened it to torture for cancer patients and cancer care providers. The interminable back and forth. The outdated fax machines. Wasting time on the phone to convince a health plan’s medical director that a cancer treatment the plan denied is the right way to go when doctors could be focused on taking care of their patients.
 Harari’s frustration with prior authorization is typical among doctors and other clinicians, who say they are increasingly burdened with onerous requirements imposed by health insurers and pharmacy benefit managers to seek advance approval for procedures and medications. They claim the requirements harm patients in the name of boosting insurers’ profits.
Harari’s frustration with prior authorization is typical among doctors and other clinicians, who say they are increasingly burdened with onerous requirements imposed by health insurers and pharmacy benefit managers to seek advance approval for procedures and medications. They claim the requirements harm patients in the name of boosting insurers’ profits.
“Cancer patients are anxious about delays and that’s what we continue to see more and more of with prior authorization: delays in getting recommended treatment underway,” said Harari, chairman of the human oncology department at the University of Wisconsin School of Medicine and Public Health in Madison.