The following are descriptions of several treatment planning research projects that our medical physicists are currently pursuing:
Introduction of 6 MV Flattening Filter Free Photon Beams (Jacqmin)
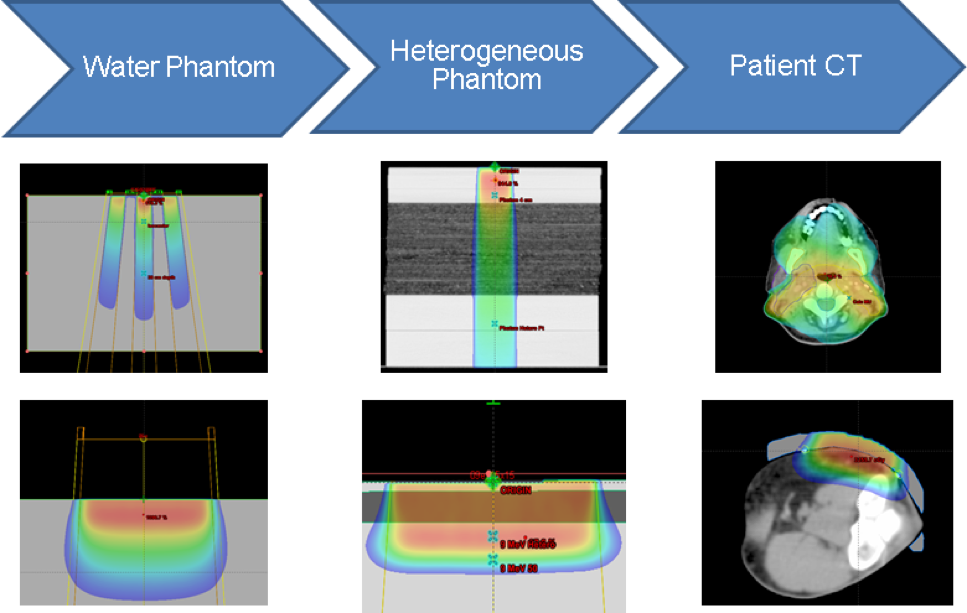
The physics team in the Department of Human Oncology has prepared a new treatment modality for fractionated stereotactic radiotherapy (FSRT) and stereotactic body radiotherapy (SBRT) on our Varian TrueBeam linear accelerators. This modality is a different kind of photon beam without a flattening filter—known as “flattening filter free” or FFF beams. Unlike the beams we have used in the past, these beams do not emerge from the machine with a uniform intensity throughout the field. This lack of uniform intensity, considered to be disadvantageous for conventional radiotherapy, is desirable for FSRT and SBRT. Even better: The removal of the flattening filter increases the dose rate up to a factor of four, allowing us to deliver these high-dose-per-fraction treatments in much less time. The physics team has worked hard to ensure that these beams are accurate for the small targets commonly treated with FSRT and SBRT.
Implementation of the validation testing in MPPG 5.a (Jacqmin)
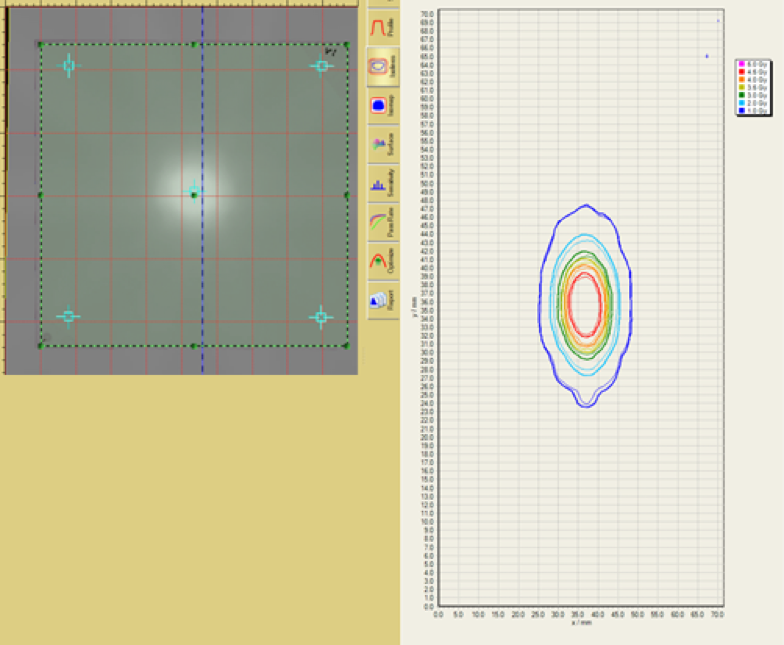
The AAPM Medical Physics Practice Guideline (MPPG) 5.a provides concise guidance on the commissioning and QA of beam modeling and dose calculation in radiotherapy treatment planning systems. We worked with physicists at multiple institutions to create a common set of treatment fields and analysis tools to deliver and analyze the validation tests in MPPG 5.a. This included the development of a novel, open-source software tool to compare scanning water tank measurements to 3D DICOM-RT Dose distributions. Dose calculation algorithms in both Pinnacle and Eclipse were tested with MPPG 5.a to validate the modeling of Varian TrueBeam linear accelerators. The validation process resulted in more than 200 water tank scans and more than 50 point measurements per institution, each of which was compared to a dose calculation from the institution’s treatment planning system (TPS). We found the use of MPPG 5.a to be a valuable resource during the commissioning process. We reported our findings in JACMP and have made our tools available to the wider physics community.
Patient-Specific Response-Informed Treatment Planning
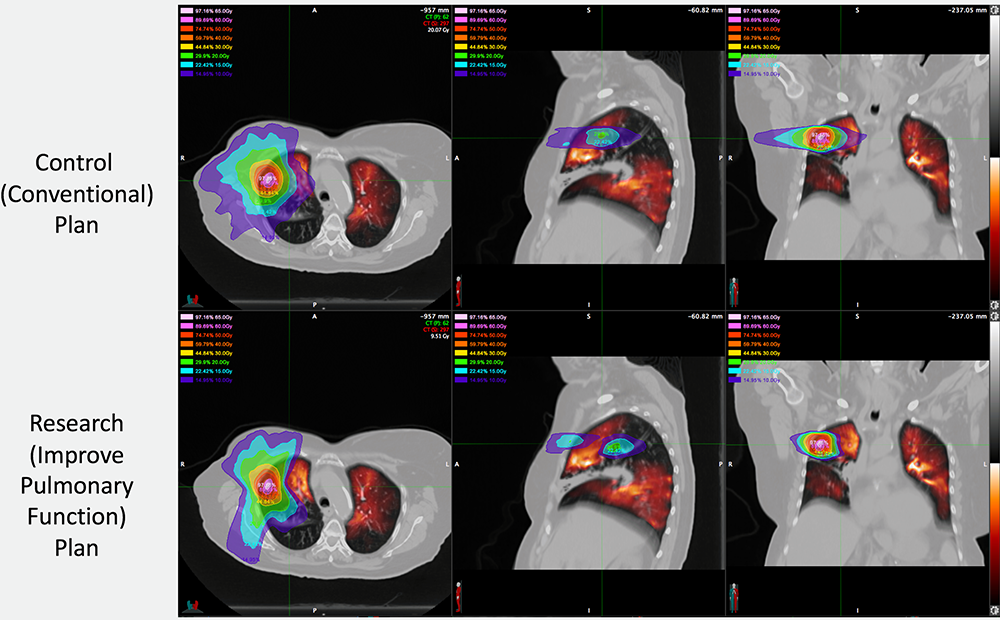
Changes to the patient occur during the course of radiation treatment, which can be eight weeks. Some of the changes are morphological (tumor size and/or position) and some are physiological (metabolic activity, inflammation, oxygenation, perfusion, etc.). We are developing imaging techniques to quantify these changes that occur during the patient’s treatment process. The results of these studies are then being used to design subsequent treatments that exploit the observed changes. This enables a new type of precision radiation therapy that we hope will significantly improve patient outcomes.
The image below shows an example of patient-specific response-informed treatment planning. This patient has highly functioning lung tissue in the apex of the right upper lobe. While this is an uncommon region of the lung to demonstrate high levels of ventilation, this knowledge enables us to design radiation treatment plans to avoid delivering doses in the high functioning lung (as shown in the second row of images). We are imaging these patients after radiation treatment as well to determine how much improvement can be accomplished using this novel therapeutic approach.
Clinical Treatment Planning System
Our problem definition is inspired by asking what we can do better with our current patients and what we would want to do if we just had the right tools on hand. Thus, significant effort is being spent on implementing a new clinical treatment planning system for patient care. This will lay the groundwork for research in adaptive therapy and improved patient modeling.
An important effort going forward is the development of medical device management techniques to manage the clinical treatment planning system. By applying modern concepts of change and state management, we are able to demonstrate system stability and calculation accuracy as we upgrade software modules or change configurations.
Non-clinical Treatment Planning System
We are implementing a second treatment planning system that closely mimics the one we are using for patient care. Within this dedicated system, we can rapidly prototype and test new planning modules and techniques. It is important that the planning system for patient care be tightly controlled and limited changes be thoroughly tested prior to use. Thus it is important to do developmental work in a separate system that can tolerate being broken and subsequent down time, but also be subject to less rigorous controls and testing.
We intend to utilize this sandbox environment to improve how we perform adaptive planning. Through the use of CT, MR and PT imaging, we are able to build three-dimensional maps of a patient’s anatomy, identifying organs and tissues. We also can create corresponding three-dimensional maps of radiation treatment dose, showing where the radiation energy is deposited. We need to extend these capabilities, to be able to do so as a patient’s anatomy changes over time, either during a single treatment course in the time-frame of weeks, or multiple courses over years. We need software and data frameworks to support this time element.
Planning unification
We employ three distinct external beam delivery technologies here at the University of Wisconsin (TrueBeam, Tomotherapy, ViewRay) in addition to brachytherapy. Each technology we use to deliver radiation dose currently has its own dedicated treatment planning system. However, each one of these systems is a data island.
Often, it is best to be able to use different delivery technologies in a single treatment course, such as boosting a prostate with HDR brachytherapy after an initial external beam treatment. It takes great manual effort to copy data between islands in order to create a plan that reflects the entire treatment course and to optimize the different plans over the treatment course. By supporting all treatment modalities within one planning environment, we can calculate and combine dose easily in order to explore the best treatment options for our patients.
Improving Treatment Plan Quality Using Data Analytics
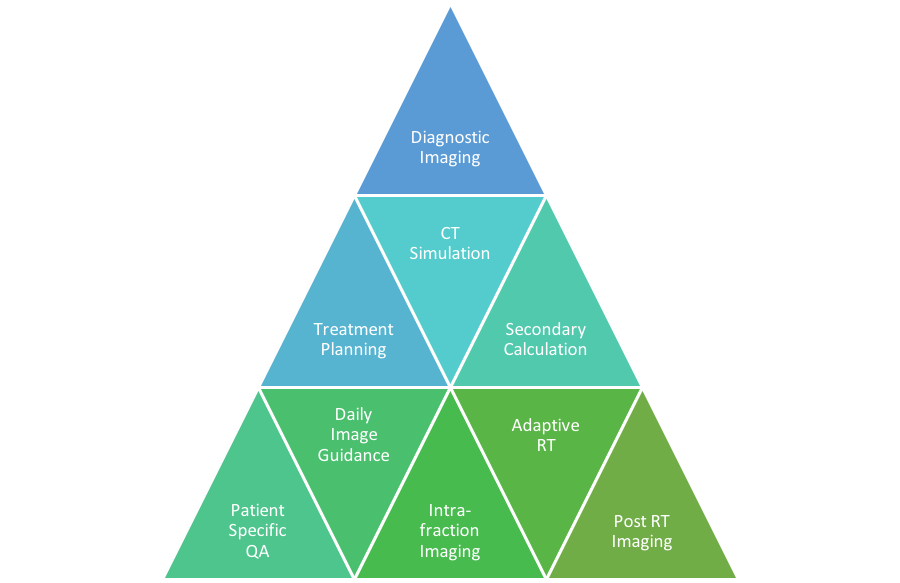
This project explores the application of data analytics to the opportunities of “big data” research into radiotherapy treatment planning and delivery. We treat more than 100 patients per day, collecting images and computing dose volumes that accumulate in the hundreds of terabytes. The illustration below highlights the many sources of data generated during modern cancer care. We are working to develop tools to scan the various data systems, study patient and plan characteristics and identify trends in plan quality. By studying the gestalt, we can identify how each individual patient is unique and better personalize our care.